Rare Disease Clinical Trials: Clinical Zoom In
June 28, 2021 Inna Grau, M.Sc. Clinical Trial ManagerRare Disease Clinical Trials: Clinical Zoom In
June 28, 2021
Inna Grau, M.Sc. Clinical Trial Manager
Over 300 million people are living with at least one of identified rare diseases around the world. Rare diseases currently affect 3.5% - 5.9% of the worldwide population. 72% of rare diseases are genetic, 70% of those genetic rare diseases start in childhood.
The fact that there are often no existing effective cures offers development products regulatory priority, this benefit together with appropriate investigational planning can lead to fast drug approval.
This newsletter covers:
- What is a Rare Disease?
- Common challenges in the choice of the study population
- Appropriate study design of Rare diseases products
- Successful efficacy evaluation in Rare diseases trials
What is a Rare Disease?
●A disease that affects a small percentage of the population. About half of the people affected by rare diseases are children. Most rare diseases are serious or life-threatening. Patients with rare diseases may have no available therapies for the disease.
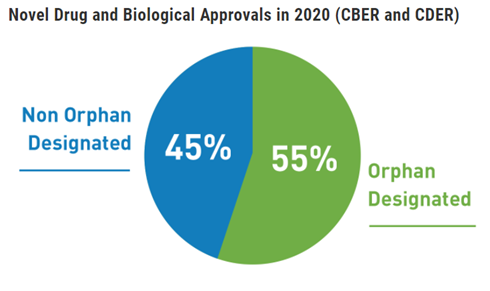
●An Orphan Drug is a drug for rare diseases. Orphan drugs follow the same regulatory development path as other pharmaceutical drugs. However, the drug can be tested on fewer patients to get approval.
The drugs for rare serious or life-threatening disorders with unmet medical needs may qualify for expedited approvals.
Regulatory priority addressed to unmet medical need
The regulations are intended to speed the availability of new therapies to patients with serious conditions, especially when there are no satisfactory alternative therapies while preserving appropriate standards for safety and effectiveness. The regulatory agency such as FDA recognizes that certain aspects of drug development that are feasible for common diseases may not be feasible for rare diseases and that development challenges are often greater with the increasing rarity of the disease.
●The agencies call for earlier attention to drugs that have promise in treating serious or life-threatening conditions.
●Encourages early consultation for sponsors to plan efficient trial design.
●Applies flexibility in situations to address particular challenges posed by each disease
How to Define the rare disease trial population
●Broad inclusion criteria can allow identification and better characterization of disease phenotypes for which therapy development may be more needed.
●The use of enrichment strategies such as demographic, pathophysiologic, historical, genetic or proteomic, clinical, and psychological characteristics can help to demonstrate treatment effectiveness.
●Choosing patients with a greater likelihood of having a disease-related endpoint event or a substantial worsening in condition.
●Choosing patients more likely to respond to the drug due to their physiology or disease characteristics and /or disease subtypes.
●Include pediatric patients with rare diseases in the study to develop data on the full range of people with the disease.
Challenges in Clinical Considerations
Sponsors developing drugs for rare diseases face many challenges. These may include the small number of disease-affected individuals, lack of understanding of the natural history of the disorder, lack of precedent for drug development (e.g., established clinical endpoints, validated biomarkers), phenotypic heterogeneity, and the need to conduct trials in pediatric populations.
●Consider the benefits and risks of the drug.
●Consider the seriousness of the disease and if there is an unmet medical need.
●Anticipated safety issues and trial stopping rules, halting rules, and patient early termination.
●Plans for an independent data monitoring committee (DMC).
●Inclusion of patient perspectives in the drug development plan.
●Plans to conduct extension studies to evaluate longer-term safety and durability of effect.
●Considerations related to novel endpoints including the development of clinical outcomes assessments e.g., patient-reported, observer reported, clinician-reported, performance outcome measures.
●Plans for pediatric studies must comply with appropriate regulatory and ethical requirements, including the additional safeguards for children.
Use of biomarkers
●Predictive biomarkers may be used for proof-of-concept.
●Drugs that are intended to be used in a biomarker-defined subtype of patients may require a companion diagnostic that shall co-development with the drug. Companion diagnostics are tests that provide information essential for the safe and effective use of a corresponding drug,
●Pharmacodynamic/response biomarkers allow guide dose-response for more precise dose-finding for therapeutic modalities. Biomarkers can be used to monitor specific parameters and adjust doses so that the biomarkers are kept within specific ranges.
●A response biomarker can be used to show that a biological response has occurred in an individual who has been exposed to a medical product, therefore, provide supportive evidence of efficacy.
Natural history-controlled studies
A natural history study is a pre-planned observational retrospective or prospective study that follows a group of people over time who have or are at risk of developing, a specific medical condition or disease. A natural history study collects health information in order to understand how the medical condition or disease develops and how to treat it. A natural history study can be submitted as a baseline, in absence of a concurrent comparator, demonstrating the disease course for untreated patients along with data that charts the disease course of patients given the proposed therapy to show how the natural progression is changed or perhaps halted by the therapy.
Retrospective natural history studies most commonly use information in existing medical records can provide quick data.
Prospective natural history studies collect and analyze new data generated from identified patients at specified time points after the natural history study has been initiated provide systematically and comprehensively captured data.
Choose sufficient study duration to capture clinically meaningful outcomes in course of the disease.
Be specific when formulating your research objectives, select potential prognostic characteristics, and disease features that may help formulate a sensitive clinical endpoint
Collect data from clinical examination findings, laboratory measurements, imaging, reports of patient functioning and feeling include the standards of care and concomitant therapies.
Include patients across a wide spectrum of disease severity and phenotypes.
Use standardized collection methods and medical terminology to enhance the value and usefulness of natural history study data.

Efficacy Endpoints
●For many rare diseases, well-characterized efficacy endpoints appropriate for the disease are not available.
●Endpoints should be selected base on the range and course of clinical manifestations associated with the disease, the clinical characteristics of the specific target population and the aspects of the disease that are meaningful to the patient and that could be assessed to evaluate the drug’s effectiveness.
●Biomarkers can be used as a surrogate endpoint that is considered reasonably likely to predict clinical benefit when analytical and clinical validation of the biomarker test is confirmed by the regulatory agency before starting the clinical trial. Endpoints that are considered reasonably likely to predict clinical benefit, even if not well-established may be used as a basis for accelerated approval for treatment of serious or life-threatening diseases.
●Exploratory evidence from phase I and II trials helps to choose the dose and timing of endpoints evaluation in the advanced stages of the clinical development program.
●When the primary endpoint is clinically meaningful but susceptible to individual interpretation, the trial may benefit from having additional supportive secondary endpoints (e.g., laboratory measurements).
●The validity, sensitivity, reliability, or interpretability of an endpoint may be different for patients with mild or severe forms of the same disease.
Efficacy vs Effectiveness
The term efficacy refers to the findings in an adequate and well-controlled clinical trial or the intent of conducting such a trial and the term effectiveness refers to the regulatory determination that is made on the basis of clinical efficacy and other data.
Studies in healthy subjects may determine which factors influence a drug’s disposition or pharmacodynamic effects, dedicated clinical trials that inform dosing and usage instructions in the target population with a rare disease may be limited. The information from such studies and analyses can inform trial design and serve as supportive evidence of effectiveness. Data generated from such studies and analyses can efficiently optimize conditions for drug use e.g., dose, schedule, patient selection, etc.
In rare disease drug development, given the limited number of available patients, it is crucial to standardize the collection and handling of data to ensure quality and interpretability.
Increased measurement variability reduces statistical power.
Safety
A smaller number of patients may be acceptable when the intended treatment population is small.
Many rare diseases are genetic in origin and characterized by more than one phenotypic subtype. Prevalence estimates should include all phenotypic subtypes of a disorder anticipated to respond to the investigational drug.
Natural history studies can help distinguish drug-related adverse effects from underlying disease manifestations.
Many rare diseases severely affect children, and for diseases that affect both children and adults, sponsors should explore the early inclusion of pediatric patients in clinical studies.
Whenever ethically and practicably feasible, to facilitate interpretation of adverse event causality, especially with respect to the incidence and severity of adverse events that could be a manifestation of the disease under study.
A trial protocol with a safety cohort running parallel to the efficacy trial would include patients with the disease who investigators think might benefit from the investigational drug but who do not meet all the registration trial eligibility criteria. Such patients can be enrolled in the trial, avoiding the need for a separate trial and protocol. However, these patients are not randomized and are excluded from the efficacy analysis.
References
●Rare Diseases: Common Issues in Drug Development Guidance for Industry, January 2019
●Rare Diseases: Early Drug Development and the Role of Pre-IND Meetings Guidance for Industry, October 2018
●Enrichment Strategies to Improve Efficiency of Drug Development, May 2018
●Guidance for Industry Expedited Programs for Serious Conditions – Drugs and Biologics, May 2014
●Patient-Focused Drug Development: Collecting Comprehensive and Representative Input, June 2020
●Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims, December 2009
●Providing Clinical Evidence of Effectiveness for Human Drug and Biological Products, May 1998
●Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims, December 2019
I●n Vitro Companion Diagnostic Devices Guidance for Industry and Food and Drug Administration Staff, August 2011
●BEST (Biomarkers, Endpoints, and other Tools) Resource, FDA-NIH Biomarker Working Group, December 2016
This Newsletter Prepared by:

Inna Grau, M.Sc. Clinical Trial Manager
For more information about our CRO services visit: